Back & Lumbar Spine Treatments
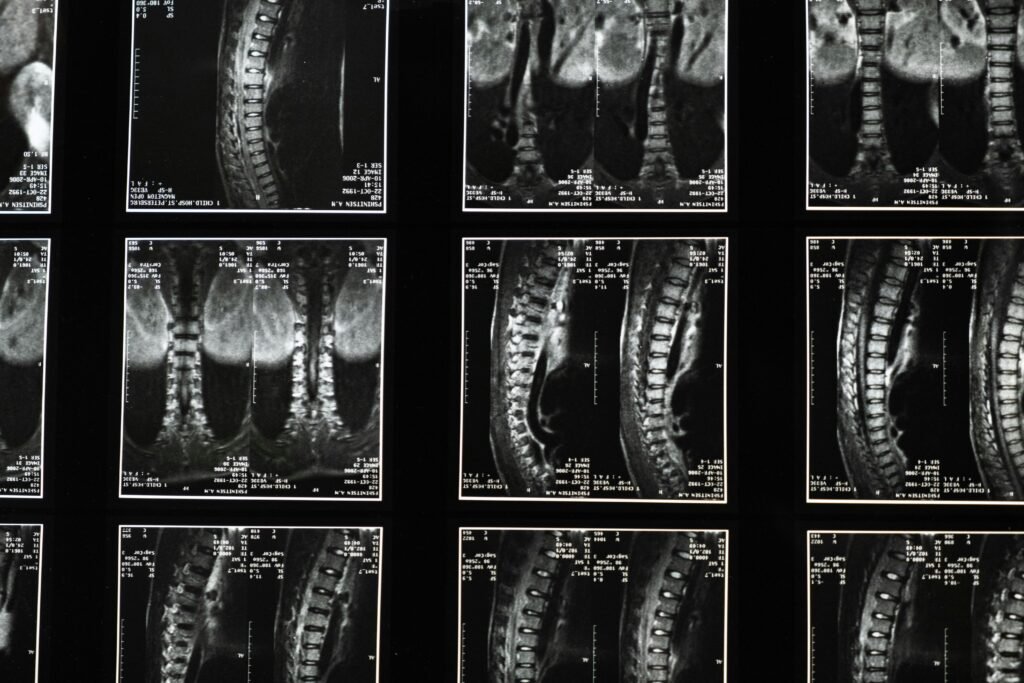
Lower back pain doesn’t always require invasive surgery. Minimally invasive options, such as epidural steroid injections, offer effective relief with less trauma and reduced post-procedure discomfort—helping you return to your daily activities faster and with greater comfort.
Living with Chronic Pain
Chronic pain is defined as pain lasting longer than three months and is different from the short-term discomfort of an injury. Its cause isn’t always clear, and it can affect not just your body but also your emotional well-being—impacting every aspect of daily life. Despite its challenges, chronic pain can be managed.
THORACIC EPIDURAL STEROID INJECTION
Thoracic epidural steroid injection is a minimally invasive procedure used for managing upper back pain from conditions such as postherpetic neuralgia, thoracic disc herniation, spinal stenosis, or facet arthropathy. By delivering steroid medication into the thoracic epidural space under imaging guidance, it helps reduce inflammation, modulate nerve irritation, and relieve neuropathic and mechanical pain. In selected patients, it provides significant pain relief, improves function, and can reduce dependence on systemic medications.
LUMBAR EPIDURAL STEROID INJECTION
A lumbar epidural steroid injection is a minimally invasive procedure designed to relieve lower back pain and radiating leg discomfort. The injection delivers steroid medication directly into the epidural space, where it reduces inflammation and swelling associated with various spinal conditions. Depending on the clinical indication, it can be administered either as an interlaminar epidural steroid injection or a transforaminal epidural steroid injection (TFESI). The procedure is typically performed under fluoroscopic (C-Arm) guidance to ensure accuracy and safety.
OZONE NUCLEOLYSIS (OZONE DISCECTOMY)
Ozone nucleolysis, also known as ozone discectomy, is a minimally invasive treatment for low back pain and sciatica caused by prolapsed lumbar intervertebral disc (PLID). In this procedure, a precise mixture of oxygen and ozone gas is injected into the affected disc under imaging guidance. The ozone reduces disc volume by dehydrating the nucleus pulposus and exerts strong anti-inflammatory and analgesic effects. This helps relieve nerve root compression and improves pain and function, offering an effective alternative to surgery in selected patients.
FACET JOINT INTERVENTIONS IN LUMBAR FACETOGENIC PAIN
Lumbar facet joints are a common source of chronic low back pain. Management options include facet joint injections with steroids or platelet-rich plasma (PRP) to reduce inflammation and promote healing. For diagnostic and therapeutic purposes, a medial branch block can temporarily relieve pain by numbing the nerves that supply the facet joint. If pain persists, radiofrequency ablation (RFA) of the medial branch nerves provides longer-term relief by interrupting pain transmission. These minimally invasive techniques are effective alternatives to surgery in well-selected patients.
RADIOFREQUENCY NEUROTOMY OF THE THORACIC/LUMBAR FACETS
This minimally invasive procedure uses heat generated by radio waves to target the nerves supplying painful facet joints in the upper or lower back. It is an effective option for patients whose pain has not improved with medications or physical therapy, providing longer-lasting relief and improved function.
RADIOFREQUENCY NEUROTOMY OF THE THORACIC/LUMBAR FACETS
This minimally invasive procedure uses heat generated by radio waves to target the nerves supplying painful facet joints in the upper or lower back. It is an effective option for patients whose pain has not improved with medications or physical therapy, providing longer-lasting relief and improved function.
SACROILIAC JOINT (SI JOINT) INTERVENTIONS
The sacroiliac (SI) joint is a well-recognized source of chronic low back pain, especially in patients with sacroiliitis or SI joint arthropathy. Under precise image guidance, SI joint steroid injections deliver targeted anti-inflammatory medication to reduce joint inflammation, alleviate pain, and improve mobility. This procedure is beneficial both diagnostically—confirming SI joint–mediated pain—and therapeutically when conservative treatments fall short. For patients requiring longer-lasting relief, radiofrequency ablation (RFA) of the lateral branches supplying the SI joint can provide extended pain reduction and enhanced quality of life.
MYOFASCIAL PLANE BLOCKS IN BACK PAIN
Myofascial plane blocks, such as the erector spinae plane (ESP) block and the quadratus lumborum (QL) block, are ultrasound-guided techniques used to manage back pain caused by muscle spasm or myofascial pain. By depositing local anesthetic (sometimes with adjuvants) in the fascial plane, these blocks reduce muscle hyperactivity, relieve pain, and improve mobility. They provide a safe, minimally invasive alternative for patients who do not respond adequately to medications or physical therapy.
HIP JOINT INJECTION
For patients experiencing hip pain, an ultrasound- or fluoroscopy-guided hip joint injection can be highly beneficial. This targeted approach not only helps your physician accurately determine the source of your discomfort but also provides meaningful pain relief, improving mobility and overall comfort.
ULTRASOUND-GUIDED PIRIFORMIS INJECTION
This procedure delivers medication directly to the piriformis muscle under ultrasound guidance to diagnose and relieve piriformis syndrome. By targeting irritation of the sciatic nerve caused by muscle contraction in the buttocks, it helps reduce pain and improve mobility.
EPIDURAL ADHESIOLYSIS / EPIDURAL NEUROPLASTY
Epidural adhesiolysis is a minimally invasive intervention designed to manage chronic back and leg pain resulting from epidural scar tissue (adhesions) that compresses or irritates spinal nerves, particularly in failed back surgery syndrome (FBSS) or degenerative disc disease. Using a specialized Racz catheter under fluoroscopic guidance, medications such as hypertonic saline, hyaluronic acid, corticosteroids, or enzymatic agents are delivered to mechanically and chemically disrupt adhesions, reduce inflammation, and restore nerve mobility. This procedure can provide significant and sustained pain relief, improve functional outcomes, and serves as an effective option for patients refractory to conventional conservative therapies.
KYPHOPLASTY / VERTEBROPLASTY
Minimally invasive procedures to treat back pain from vertebral compression fractures due to osteoporosis, trauma, or malignancy. Cement injection stabilizes the vertebra, providing rapid pain relief, improved mobility, and spinal support.
GANGLION IMPAR BLOCK
A ganglion impar block is a precise, minimally invasive procedure used to manage chronic perineal, coccygeal, or pelvic pain, often arising from cancer, trauma, or post-surgical conditions. By targeting the ganglion impar—the nerve cluster at the base of the coccyx—under imaging guidance, this block interrupts pain signals, providing significant relief, reducing the need for opioids, and improving patient comfort and quality of life.
REGENERATIVE MEDICINE IN BACK PAIN
Platelet-Rich Plasma (PRP) is an emerging regenerative therapy for managing chronic back pain by promoting tissue healing and modulating inflammation. PRP can be delivered into facet joints, sacroiliac joints, intervertebral discs, or myofascial planes to target facetogenic pain, sacroiliitis, discogenic pain, and myofascial/back muscle pain. These injections offer a minimally invasive option that supports tissue repair, reduces pain, and may improve function in patients who have an inadequate response to conventional conservative or interventional therapies.